University of Canterbury researchers have made progress in developing effective treatments for children and adolescents on the autism spectrum who have sleeping problems.
Lead investigator of the Good Nights Canterbury and Autism Sleep project, Dr Laurie McLay, tells to Jesse Mulligan consistency is key when bringing improvements to a child's sleep patterns.

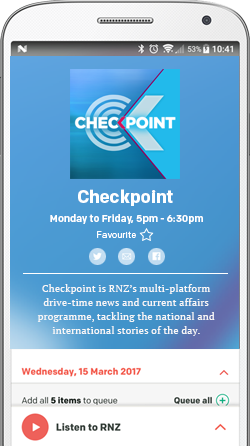
Photo: supplied
She says her organisation works with a variety of adolescents experiencing sleeping problems.
"Their problems vary greatly actually, from issues with sleep onset, difficulties getting to sleep, difficulties staying asleep, early morning waking, there’s co-sleeping issues that parents would like to address and anxiety around sleep," she says.
The impact on families can be significant.
“We know that chronic sleep deprivation and interruption has an impact on children’s learning, their day-time behaviour, social interaction and all of those kinds of things. In addition to that it has an impact on the mental health and wellbeing parents, their ability to work and all sorts of secondary effects.”
The support systems for families with autistic children haven't really addressed the subject in great depth. She says her work came about from them working with autistic children and their families because sleep was being raised as a common problem.
“Around 40-to-80 percent of children on the autism spectrum experience some type of sleep problem. So, based on my experience and some of the work of my colleagues… we came together and started our work in this area.
“Typically, what we see is that sleep problems, prior to the work we were doing, were treated with medication, mostly with melatonin.
“We were really interested in applying some of the strategies that have been used with good effect with infants and young children who are typically developing, looking at whether there are environmental things we might be able to change that would make a difference with children with ASD.”
One of the key principles of the approach is to treat each child in a unique way and this reflects varying types of treatments offered. Each child is assessed rigorously, McLay says.
“Usually we start with changes we might be able to make to circadian factors – looking at getting consistently around sleep-wake times and ensuring that bedtimes are developmentally age-appropriate.
“Then we look at some of the environmental factors that may be playing a part. We refer to it as sleep hygiene, making sure that the bedroom is sufficiently dark, quiet, warm… Looking at the conditions in which kids are falling asleep and whether these are consistent throughout the night.”
One common condition that affected sleep was when a child fell asleep with a parent present and then woke up later to find that parent absent.
She also looks at how the parents are responding when children are having difficulties getting to sleep and what that child may be accessing during that time – whether it’s snacks, water or devices.
“It’s really identifying why the child isn’t sleeping and coming up with an individualised plan based on that information.”
The results have been good, she says. The research recent paper looked at 40 children and it showed the modifications led to significant improvements in all the various sleep problems looked at.
McLay says the key principles of consistency and conditions would help any parents with autistic children improve sleep patterns.