The chief ombudsman says the mental health ward at Palmerston North Hospital is one of the worst in New Zealand and not fit for purpose.

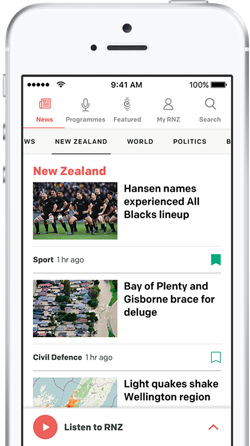
Photo: RNZ / Jimmy Ellingham
In a damning report, released on Monday, Peter Boshier urges officials to get on with building a replacement ward that has already fallen behind schedule.
The ward was ruled below par after two suspected suicides of patients there in 2014.
Five years later the government announced it would be replaced, yet the new $35 million facility remains in the planning phase and, as RNZ yesterday revealed, is not expected to open until late 2023 at the earliest, a year later than expected.
Boshier told RNZ the layout of the present ward, which he described as one of New Zealand's worst, was poor.
"It's sterile and institutional. There's no physical separation between male and female parts of the ward. The high-needs unit is stark, noisy and crowded.
"There's not enough natural light in the high-needs unit and no access to fresh air from the seclusion rooms, as well as a lack of privacy."
Boshier issued 17 recommendations to improve the ward. All have been accepted by the MidCentral District Health Board.
Among them are reducing the disproportionate use of seclusion for Māori; allowing patients to make written complaints independently of staff; doing maintenance and urgent repair work in the high-needs-unit; urgently progressing the new ward; ensuring there is adequate staffing and that all staff training is up to date.

Peter Boshier made 17 recommendations to improve the ward. Photo: RNZ /Dom Thomas
Boshier found the ward was at or over its 28-bed capacity and there were not always adequate numbers of staff working. Staff members sometimes had not received all the training they required.
The inspection was a random one, in May 2021, to make sure the ward is abiding by New Zealand's international human rights obligations against torture.
"When you have a unit that's not fit for purpose and the result of that has caused a lot of distress to some families you are not reaching the requirements of international standards," Boshier said.
"I'm sad that New Zealand is in this position...
"No-one can predict, necessarily, when they might have a mental illness which needs acute admission.
"I'd think that we would say to someone in that position: 'You will get the best, dignified, civilised setting possible to get you better', yet in this case, if you're unlucky enough to come into ward 21, it looks to me as if you're not going to."
As he has done with other institutions, Boshier highlights that Māori patients are disproportionately more likely to be placed into seclusion at ward 21.
It is a nation-wide problem he said needed fixing, although the overall rate of seclusions at the Palmerston North ward was dropping.
At ward 21, 78 percent of seclusions were for Māori patients, yet they made up 38 percent of those on the ward.
The high-needs units came in for special focus, and urgent corrective work was required. Among the problems was graffiti, including a swastika, on the bedroom doors.
Carey Hume's daughter Erica died in a suspected suicide on the ward in 2014.
Carey Hume said she and husband Owen wanted to see the ombudsman's recommendations immediately implemented.
"I want [MidCentral] to put into place auditing procedures of these many items to ensure that any slippage in policies and procedures, and supply of services or care, is caught early and stopped in its tracks.
"To not do so directly impacts on the care given to the mental health patients within ward 21 at a time they are most in need," Hume said.
"To not do so also sends the message that Palmerston North Hospital-MidCentral do not care about their mental health inpatients, which I truly hope is not the case. Their actions will show us which is true."
She was disappointed to see problems raised in previous reports, such as inadequate staffing, come up again.
Also in 2014, Shaun Gray died in a suspected suicide on the ward.
His brother, family spokesman Ricky Gray, said the ombudsman's report showed patient care on the ward was not improving.
"The key callouts from the report are medication errors, seclusion errors, maintenance not being conducted, and inadequate training of staff.
"The key things for us is these are all factors that contributed to Shaun's death. Seeing them eight years later is a disgrace."
MidCentral DHB operations executive, Te Uru Rauhī - mental health and addiction Scott Ambridge said although improvements were needed, it was good to see that overall patients were positive about their treatment, care and relationships with staff.
In a statement, he said the report was a "useful tool to help us see where we can improve, and as the ombudsman said, we accept all his recommendations and will be imbedding them into our approach".
MidCentral aimed to eliminate seclusion and was working with its staff to achieve that. "We still have a way to go on this and are taking it very seriously," Ambridge said.
In April only one patient was placed into seclusion and there was a 20-day stretch when there were none.
"The ombudsman identified there were some gaps in our staff training, which we have now largely addressed.
"At the time, we had several new staff, thanks to our recruitment efforts, and other staff who were on long-term leave from the ward. We also had some staff where in-person training had been deferred due to Covid-19 interruptions."
Ambridge said the new ward was "our most crucial priority", and MidCentral had identified improvements to the present high-needs unit.
"We've already installed $20,000 worth of new soft furniture and furnishings for the [unit], and these items will also be able to be used in our future facility."