Differing pay rates for nurses is causing a crisis in rest home care, as more and more of our population requires it.

Photo: Photo / 123RF
New Zealand has a nursing pay inequity, and it's fuelling a rest home crisis - which is in turn holding up hospital waiting lists.
Rest homes are closing hundreds of beds thanks to a shortage of nurses, who are looking over at their Health NZ counterparts being paid 20 percent more.
"[The agreement is] yet to be ratified," says New Zealand Aged Care Association deputy chair Warick Dunn, "but it's expected to, and that will open up a big financial gulf between the sectors."
Several other factors complicate the problem.
Foreign nurses that the aged care sector relies heavily on aren't part of the new fast-track residency scheme, so can't be enticed in that way.
Covid means elderly people are "bed-blocking" public hospitals, which are then not available for elective surgery.
Rural areas and the regions are particularly struck because they don't have large retirement villages to cross-subsidise wages.
And our population is rapidly aging. Today we have 83,000 people aged over 85. In 2050, that number will be 383,000.
Today on The Detail, Emile Donovan looks at how the aged care sector is structured in New Zealand, what the advantages and vulnerabilities are, and what could help to arrest this decline.
"Past generations used to have three generations living in a house," says Dunn.
"But changing expectations, things like women working, household finances requiring two people to work, has meant the state has recognised the need to have a specialised area of care for older people. And the reality is that the type of care that folk need, particularly towards the end of their life, really is not being able to be provided by family members."
That recognition by the government means that healthcare providers get some funding, allocated on the basis of the type of care needed - be it hospital, dementia level, or rest home care.
But Dunn says it doesn't go anywhere near covering the complex needs of most elderly patients. Charitable aged care providers and smaller operations are closing down.
"Where do these folk go? There's no capacity left in the sector so they end up staying in hospital, bed-blocking, and the consequences of that is that if you or I have a pre-planned hip joint or knee replacement to be done we can't go in ... because there are no beds, there are no nurses, they're caring for the older person who should be, rightly, in the aged care sector where specialty care is available.
"I think aged care will become a pretty scarce resource. And sadly the people who will bear the cost of that, disproportionately, are those folk who arrive at their latter years without capital, and probably only surviving on the state pension.
"Unless the sector is better supported, I don't know what is going to happen to those folk."
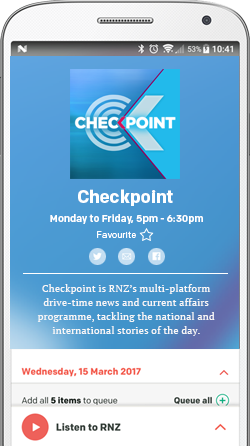
Find out how to listen and subscribe to The Detail here.
You can also stay up-to-date by liking us on Facebook or following us on Twitter.

Photo: