Pain is a universal human experience, yet we understand very little about the mechanics of it.
As a result, our treatments are still fairly rudimentary, says pain medicine specialist Dr Abdul Lalkhen.
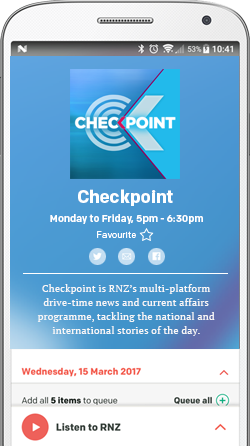
His new book Pain: The Science of the Feeling Brain is for people who struggle to manage their own.

Photo: Road Trip with Raj / Unsplash
The nature of an individual’s pain needs to be understood from the outset, Dr Lalkhen tells Kathyrn Ryan.
“The way to think about pain is, it’s an experience. We talk to one another and somebody says, 'oh I’ve got pain' and there is an assumption we automatically know what that person means.
"It is a unique experience and whilst the biology and bits of our body used to detect damage are pretty much the same, when those signals reach the brain they are interpreted through our unique cognitive and emotional framework to produce that experience of pain. Using pain merely as a guide to disease is often misleading because of the different way that it is expressed.
“Pain and suffering are intimately linked, but they’re not necessarily the same. I think it’s also important to distinguish between the pain from damage – if you step on a drawing pin and damage the skin the brain needs to know about that problem because obviously if you didn’t attend to it then it could get infected and it would threaten the organism. That’s a simple kind of brain problem, which is usually resolved by removing that drawing pin.
“But when things become more complicated and long-term – for example, if you have diabetes and your nerves are damaged as a consequence of diabetes, the body then reactions by producing abnormal sensations all of the time, rather than the drawing pint, which is time-limited and that requires a different approach in terms of managing that pain alarm.
“The same is true with conditions like arthritis and more widespread conditions like fibromyalgia and lower back pain, which we don’t fully understand, but we’re certain normal biological alarm systems malfunction.
“We try to apply simple solutions to those complex problems, often with deleterious results to the person. We kind of throw a blanket over those signals by giving people opioids but that then leads to further changes in brain chemistry, which cause further problems."
Some people experience a 'pain alarm system' going off all the time but not flagging actual damage to the body, Dr Lalkhen says.
That alarm may seem a lot 'louder' when there is a stressor in their environment, such as a domestic row or a work-related dispute.
Modern medicine’s approach to pain modulation has a place in treatment, but risks need to be weighed up against benefits, he says.
“The reality is the alarm is pretty much the same all the time, but it is your response to it [that fluctuates]. Living well with chronic pain is really about learning to understand that process. And for a doctor to say, ‘I can perhaps reduce the volume of that alarm, the problem is the drugs I may use may also have side effects, and you, therefore, learning how to pace your activities or avoid stressful situations that make that alarm louder, that is another way of learning to help yourself cope with persistent pain.”

Photo: Pixabay / Supplied
Explaining the nature of pain to patients helps reduce the fight-or-flight state of worry about what it may be signalling, Dr Lalkhen says.
This allows the person to relax and reinterpret their pain as something they can more easily cope with.
Acute pain can be a huge challenge to treat, though, he says.
“I completely understand there are times when the pain is intractable and severe but there should always be an attempt made to try and have the individual understand the problem. That’s not easy and sometimes patient’s push against it because they just want a simple solution.
“But in my experience, unless you have that conversation and people are able to move to that point where they understand the problem, that is why they’re experiencing that severe and intractable pain and they’re expressing that degree of distress is simply an inability or not having had the issue had clear, or really struggling psychologically to come to terms with what they’re feeling.
"And if you just respond to their distress - which is a perfectly normal human response - with medication, that’s where it tends to lead to the escalation of [opioid use] for example, with really quite disastrous effects long-term.”
Support, empathy, caring and compassion play an important role in recovery from longer-term pain, Dr Lalkhen says.
“All pain aspects require a holistic, biological, psychological and social approach if they are to be managed appropriately, and really that’s what the book is aimed at – to try and unpack all that and try and help people understand what it is they’re going through.”
The basic physiological function of pain involves a signal to the brain that the body is in danger, and as such anything that threatens us will lead to an unpleasant physical experience, he says.
When we stand on a drawing pin, a system of pain is triggered, first by localised inflammation releasing chemicals.
"Those chemicals attached to nerve endings that have specific receptors called non-receptors… so that mechanical damage of the drawing pin is converted into an electrical signal from your peripheral nerves to your spinal cord, which is a sort of junction box.
"Those messages are then relayed, and if you imagine fireworks going off in the night sky different parts of the brain and they go to the parts of the brain that deal with the where, the what have I experienced before, how am I interpreting it in that context, and so the brain perceives that there’s a problem and the brain then decides how important this drawing pin is – this injury, what does it mean. It can then increase the number of signals to the brain or decrease it. So, the experience of pain is produced in the brain as a consequence of that system.
"Now, usually once you take the drawing pin out and the foot heals, those chemicals are no longer present and the nerves are no longer stimulated so the signalling stops and in time the pain stops.”
When that system goes wrong, people develop chronic pain which persists in the absence of ongoing tissue damage.
In the case of a mechanical problem like a slipped disc compressing a nerve, the pain caused by the distortion of the nerve, as well as the inflammation produced as a result of the compression, may remain even after successful surgeries due to nerves being sensitised.
Managing this kind of persistent pain can involve medications and a spinal cord stimulator, which can put a break on nerves that are hypersensitive.
Treatment of conditions like fibromyalgia, where the body's pain alert system is constantly on, must take a holistic approach, Dr Lalkhen says.
"It really starts with education. It starts with what chronic pain is and it doesn’t rely on ongoing damage. Most people get into a cycle where their understanding is that pain is due to damage, therefore if I did more, and I had more pain, I’m doing more damage they then stop moving, which makes muscles and joints stiff and when they do move they get pain and they end up getting caught in this cycle of distress and disability.
“Breaking that cycle involves understanding the condition and then supporting [the person] to rehabilitate it by teaching them how to manage that pain.”
Dr Abdul Lalkhen is a member of the Faculty of Pain Medicine at the Royal College of Anesthetists in the UK and a visiting professor at Manchester Metropolitan University.